First things first how do you pronounce this rare disease? Here it goes… Con-gen-ital Hyper-in-su-lin-ism! Whew! 😰 It really is a mouthful, when you put it all together.
You wonder why I’ve been hiding under the “type 1 diabetes” umbrella for so long? It was partly and shamefully because, I couldn’t pronounce it🤦🏾♀️. It was easier just to explain my journey rather than actually name the condition but, how can I raise awareness, and even connect with others with the similar experience to me?
So, if you have read my first post discussing my journey with diabetes, “Diabetes & I” I explain how I was born premature with a pancreas that over produced insulin. In a nutshell that is what Congential Hyperinsulinsim (CHI) is, a rare disease that causes the pancreas to over produce insulin.
Hyperinsulinsim (HI) affects around 1 in 28,400 babies in the UK and Ireland, it is usually present during the neonatal, infancy and childhood stage.

The pancreas is an organ in the body which produces insulin – a hormone which controls the levels of sugar in your blood. The pancreas is also vital to digestive functions, it produces enzymes which breaks down food.
A hypo or low blood sugar level is anything below 4mmol.
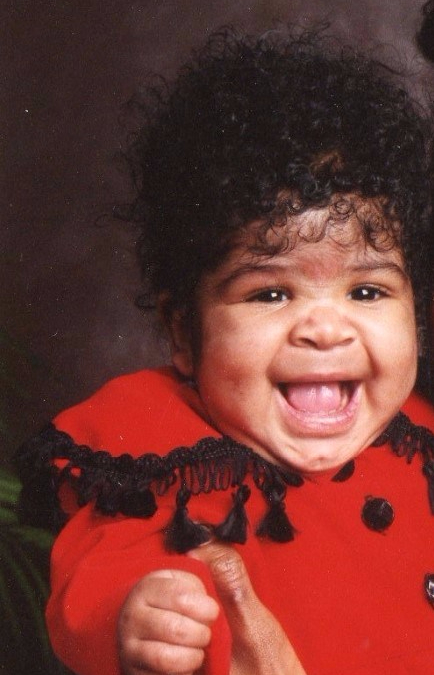
My pancreas was overproducing insulin, more than what an adult would be able to manage never mind a new-born baby. This caused extremely low blood sugar levels when I was born which meant that I spent the first 6 months of my life in hospital, as the amazing Doctors looked to treat this condition.
Due to being born in the 90’s the treatments for CHI wasn’t as advanced as what I know them to be now. I was given various treatments such as steroids and also was given a feeding tube. This was to help treat the consistent hypos that I was having.
The treatment methods only helped to suppress the insulin production slightly but, there were side effects namely the steroids caused me to gain facial hair around my forehead and sideburns.

Despite the extensive treatments I was still experiencing hypos so at 4 months old I underwent surgery to remove 95% of my pancreas. This is a common treatment of CHI especially at the time, in some extreme cases the entire pancreas is removed.
Even with having only 5% of a pancreas I was still experiencing low blood sugars so I remained on a feeding tube to help. I had a nasal feeding tube up until the age of 2 before upgrading to a feeding tube in my stomach until the age of 8.

During this time I monitored my blood sugar levels via finger pricks, and was under a General Paediatric outpatient care. When I turned 9 I was transferred to a Children’s Diabetic clinic as I had hit the pubescent stage, the 5% pancreas ironically wasn’t producing enough insulin for my growing body. As a result, I was put on insulin injections, it was at this point I consider being officially “diagnosed” with diabetes.
At the Paediatric outpatients they had told me that I may need enzyme therapy due to not having a complete pancreas. Luckily, I have not had to have this although since transferring to the diabetic clinic the health of my little pancreas has been overlooked.
As you can see my diagnosis story is not the same as your usual type 1 diabetic, however, my medical records state that I have type 1 diabetes, and for sometime I have just accepted that title. Interestingly enough, in the USA they would say that I have type 3c diabetes.
To be really honest, as crazy as it sounds, I feel some form of imposter syndrome & guilt for accepting the type 1 diabetic label. I sometimes feel that I am taking up space within the type 1 diabetes community. Especially when I can’t relate to diagnosis stories etc (I know it sounds crazy!).
The typing system of diabetes can be so confusing, but what I do know for certain is that I have diabetes. If I were to put myself into a category I personally would say I have ‘secondary type 1 diabetes’. This is because I was made diabetic as a result of having the majority of my pancreas removed.
Diabetes “cured” my Congenital Hyperinsulinism. Diabetes saved my life.
🚨IMPORTANT!🚨
Consistent hypos can cause neurological harm. Knowing the signs of a hypo in a baby is crucial and can save a life.
How to spot the signs of a hypo in an infant
- Headaches
- Dizziness
- Weakness/tiredness
- Confusion
- Changes in behaviour
- Paleness
- Tremors
- Shakiness
- Sweating
- Breathing problems: pauses in breathing, rapid breathing
- Blurred vision
- Seizures
- Irritablity
- Poor feeding or vomiting
- Problems keeping the body warm
This list is not exhaustive and some children do not show symptoms but, it’s always good to be aware of the signs.
Thanks to the power of social media I have come across people who like me, have undergone a pancreatamoy and are now living with diabetes today. There is also useful pages online dedicated to this condition, @chi_hypoglycemia & @chcharityuk.
For families affected by CHI here are links for support… www.hyperinsulinsm.co.uk and www.congentialhi.org
I hope to connect with more people affected by CHI so if you’re reading this now please share via the links below. Help me to spread awareness of this rare condition!
Feel free to share your thoughts in the comments also!
Before you go, here is a bitesize video of my journey from CHI to Diabetes.
Thanks for taking the time to read 😊.
khadija mary 🤍




Leave a comment